What is Crohn’s Disease?
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that leads to long-lasting inflammation in the digestive tract, resulting in symptoms like abdominal pain and diarrhea. Unlike some other gastrointestinal disorders, Crohn’s disease can affect any part of the digestive system from the mouth to the anus, though it most commonly occurs in the terminal ileum, where the small intestine meets the large intestine.
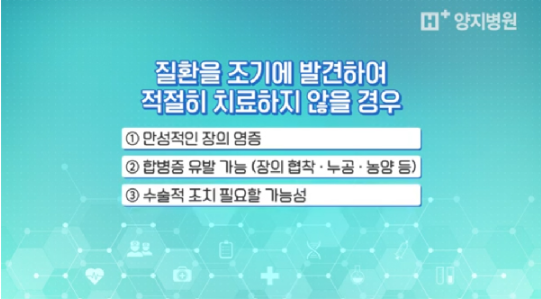
If left untreated, Crohn’s disease can lead to:
- Persistent inflammation in the intestines
- Complications such as strictures (narrowing of the intestines), fistulas, or abscesses
- The need for surgical intervention in severe cases
Causes of Crohn’s Disease
The exact cause of Crohn’s disease remains unknown, but it is believed to result from a combination of environmental factors, genetic predisposition, and an overactive immune response to the natural bacterial flora in the digestive tract.
Symptoms of Crohn’s Disease
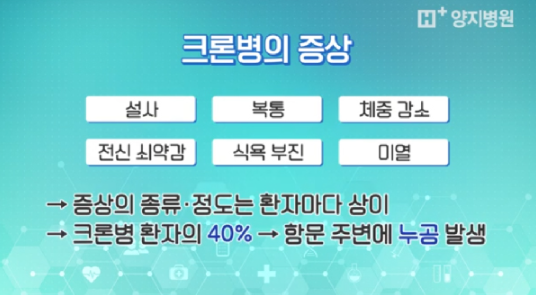
Common symptoms of Crohn’s disease include:
- Diarrhea
- Abdominal pain
- Weight loss
- Fatigue
- Loss of appetite
- Low-grade fever
About 40% of Crohn’s patients may also develop fistulas around the anus. Symptoms can vary significantly depending on the individual, with some experiencing mild discomfort while others face severe, life-impacting symptoms.
Diagnosing Crohn’s Disease
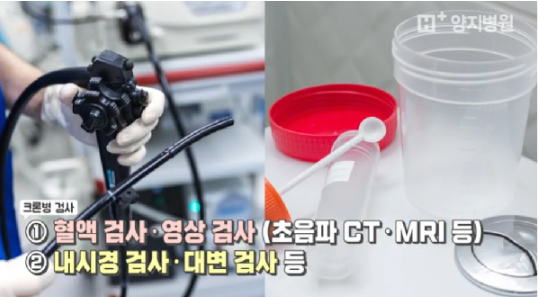
Diagnosing Crohn’s disease requires a comprehensive approach as no single test confirms the condition. Diagnosis typically involves:
- Medical History Review: Understanding symptom patterns and family history
- Blood Tests and Imaging: Tests like ultrasounds, CT scans, and MRIs help detect inflammation or abnormalities.
- Endoscopy and Colonoscopy: Essential procedures for visualizing the intestines and performing tissue biopsies.
- Stool Tests: To rule out infections and check for inflammation indicators.
A diagnosis is made by combining results from these tests and the patient’s symptoms.
Treatment Options for Crohn’s Disease
The primary goals of Crohn’s treatment are to induce and maintain remission, improve quality of life, and prevent complications. Treatment varies based on the disease’s activity level, affected area, and specific characteristics of the condition.
- Medications: Include anti-inflammatory drugs, corticosteroids, immunomodulators, antibiotics, and biologics.
- Surgical Intervention: Surgery may be necessary if:
- Symptoms do not respond to medication
- Complications like severe bleeding, persistent intestinal obstruction, colorectal cancer, abscesses, or fistulas arise.
Each treatment plan is personalized, aiming to manage symptoms effectively and prevent flare-ups, thereby helping patients lead fulfilling lives despite the chronic nature of the disease.
 +84 24-7306-9889
+84 24-7306-9889  Booking
Booking